Call to speak to a Licensed Insurance Agent
Mon - Fri 8am – 8pm EST; Sat - Sun 10am - 6pm EST
Do you want to know if Medicare will pay for pelvic floor therapy? Most times, the answer is no.
But sometimes, there are special cases where it might. This article is going to talk about those special cases. We’ll also look at what the basic Medicare and Medicare Advantage plans usually say about paying for this type of therapy.
If you’re having problems with your pelvic floor and are thinking about getting therapy, it’s good to know how much of the bill Medicare might cover. This can be really important if this health issue is messing with your day-to-day life.
What you’ll learn in this article:
Keep reading if you want to learn all the details about how Medicare deals with pelvic floor therapy.
The short answer is no. In most cases, Medicare will not cover the cost of pelvic floor physical therapy. That said, there may be some situations where you can get these costs covered. Below we’ll take a closer look at this to see when you might be able to get Medicare to pay for your pelvic floor physical therapy.
Original Medicare (Medicare Part A and Part B) does not provide coverage for pelvic floor physical therapy. The main reason why Original Medicare does not provide this coverage is because it is not considered medically necessary.
However, Original Medicare provides coverage for general physical therapy (PT) if it is medically necessary. Your healthcare provider must first order the operation for Original Medicare to provide coverage.
Coverage for physical therapy is provided by Medicare Part A if it takes place in an inpatient setting. Medicare Part A will cover 100 percent of the costs of hospital stays for up to 60 days.
For days 61 to 90, Medicare Part A will still provide coverage. However, you will pay a copayment each day you are in the hospital. After 90 days, Medicare Part A will no longer provide coverage.
However, Medicare Part A provides 60 lifetime reserve days. If you have them, they will still provide coverage for your hospital stay after 90 days. But you will be charged a daily copayment.
Coverage for therapy is provided by Medicare Part B if it takes place in an outpatient setting. Once approved, Medicare Part B covers 80 percent of physical therapy costs. You will pay for the remaining 20 percent.
Like Original Medicare, Medicare Advantage plans (Medicare Part C) do not cover pelvic floor physical therapy. Medicare Advantage plans have to cover everything Original Medicare covers.
But these plans offer additional benefits as well. However, what these plans will cover and how much this coverage costs will vary from plan to plan.
Pelvic floor physical therapy usually costs around $225 for the initial session and about $180 for each 45-minute follow-up session.
You may get coverage if you have specific conditions such as urinary incontinence or pelvic organ prolapse. But you’ll first need to try other treatments first. For potential coverage, you’ll need to:
If Medicare denies your claim, you can appeal the decision. If that happens, you might want to:
For more help, you can check out Medicare’s own website. You can also talk to your state’s office that deals with insurance or look for non-profit groups that might help you understand costs better.
Also, check out if you may qualify for any grants to help pay for your treatment.
Don’t forget, you have other options to help you pay for the therapy too. You can use your own health insurance if you have it, ask your job if they offer any help, or even look for local groups that might offer some support.
In addition to the previously mentioned resources, other financial assistance options may be available:
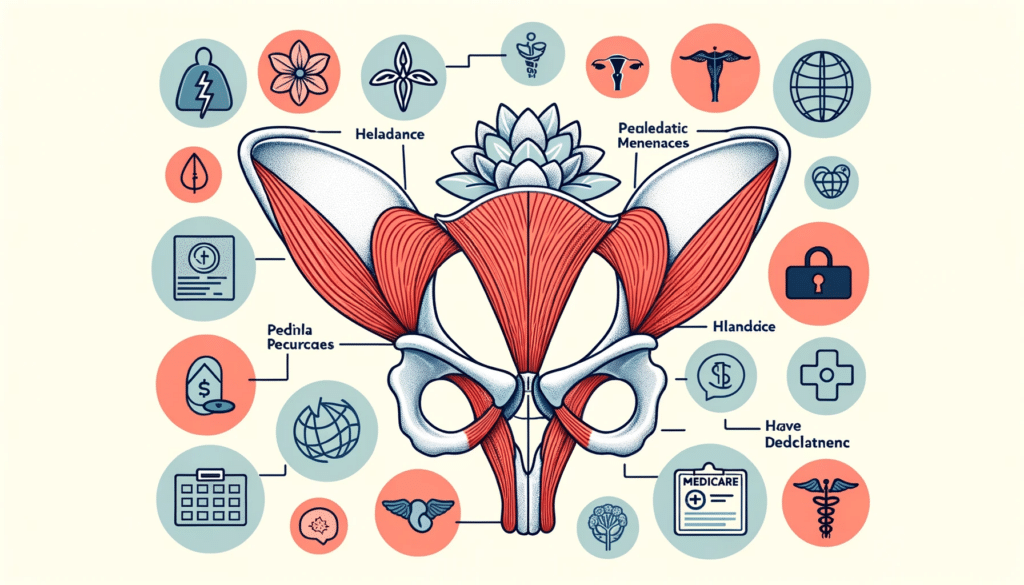
Pelvic floor therapy focuses on strengthening or relaxing the muscles at the bottom of your pelvis. These muscles help support important organs like the bladder and bowel, and they also play a part in sexual function.
The pelvic floor consists of a group of muscles located at the base of the pelvis. These muscles serve three primary functions: they provide support to the pelvic organs, assist in regulating urination and defecation, and play a role in sexual activities.
Pelvic floor therapy is utilized for a variety of conditions. These conditions can range from stress urinary incontinence (SUI) and urge urinary incontinence (UUI) to constipation and pelvic organ prolapse.
Additionally, the therapy can be used for issues related to pain during or after sexual activities. Other conditions that may be treated through pelvic floor therapy include painful bladder syndrome, vaginal dryness, and pelvic floor muscle dysfunction.
Opting for pelvic floor therapy can significantly enhance the performance of your pelvic muscles, offering you better control over various symptoms. Not only can this therapy alleviate existing issues, but it can also prevent them from worsening as time goes by.
The pelvic floor muscles have the function of supporting pelvic organs and managing urination and bowel movements. Additionally, they play a role in sexual function. Issues such as incontinence, constipation, and pain may arise when these muscles are either too weak or too tight.
Problems with your pelvic floor can really affect your quality of life. You might find everyday activities like walking or sitting uncomfortable. It can also mess with your sexual life and relationships.
In pelvic floor therapy, a variety of techniques are commonly employed. These include education and counseling to inform you about pelvic floor anatomy and function, as well as exercises to strengthen or relax these muscles.
Biofeedback uses sensors to monitor pelvic floor muscle activity, aiding in muscle control. Electrical stimulation applies mild electrical currents to either strengthen or relax the pelvic floor muscles.
Manual therapy involves hands-on manipulation of these muscles by the therapist. Finally, exercises are taught to further assist in strengthening and relaxing the pelvic floor muscles.
Above, we looked at whether Medicare will help pay for pelvic floor therapy. We looked at what the basic Medicare plan and the upgraded Medicare Advantage plans usually cover. We also talked about how much you might have to pay yourself for this kind of therapy.
We gave some tips on the special cases where Medicare might help cover the costs. Knowing what Medicare will and won’t pay for can be really important if you’re dealing with pelvic floor issues that affect your everyday life. Being in the know about what help you can get is really useful.
If you think this article was helpful, you might want to share it with other people who are also trying to figure out Medicare and pelvic floor therapy. It’s a tricky subject, so spreading the word can help others too.
If you experience bladder issues, pelvic pain, or discomfort during sexual activity, pelvic floor therapy might be a beneficial option for you. This treatment addresses various pelvic floor conditions and can provide valuable insights into bodily functions. The therapy aims to improve core strength, rehabilitate pelvic floor muscles, and manage symptoms like leakage.
If you face challenges such as bladder issues, pelvic pain, or discomfort during sexual activities, pelvic floor therapy may be a suitable option. The therapy focuses on strengthening pelvic muscles to address symptoms like leakage. It is used for a range of conditions including frequent urination, constipation, and pelvic pain.
It is never too late to begin pelvic floor exercises. These exercises are applicable for women of all ages and are not solely beneficial after childbirth. While starting early is advantageous, initiating these exercises at any stage is effective for preparation for future health concerns or for addressing existing conditions.
Pelvic physical therapy might sound strange or uncomfortable, but it usually works well. Many people feel better and enjoy life more after treatment. How well it works can depend on how serious the condition is.
Note: Medicare coverage changes all the time. And your specific coverage may vary from plan to plan for Medicare Advantage. Always be sure to double-check with your health care provider and/or Medicare insurance provider about what your plan covers and what it does not.
Also, you can check out other articles in this series, including does Medicare cover Boniva and about Medicare coverage for shock wave therapy.