Call to speak to a Licensed Insurance Agent
Mon - Fri 8am – 8pm EST; Sat - Sun 10am - 6pm EST
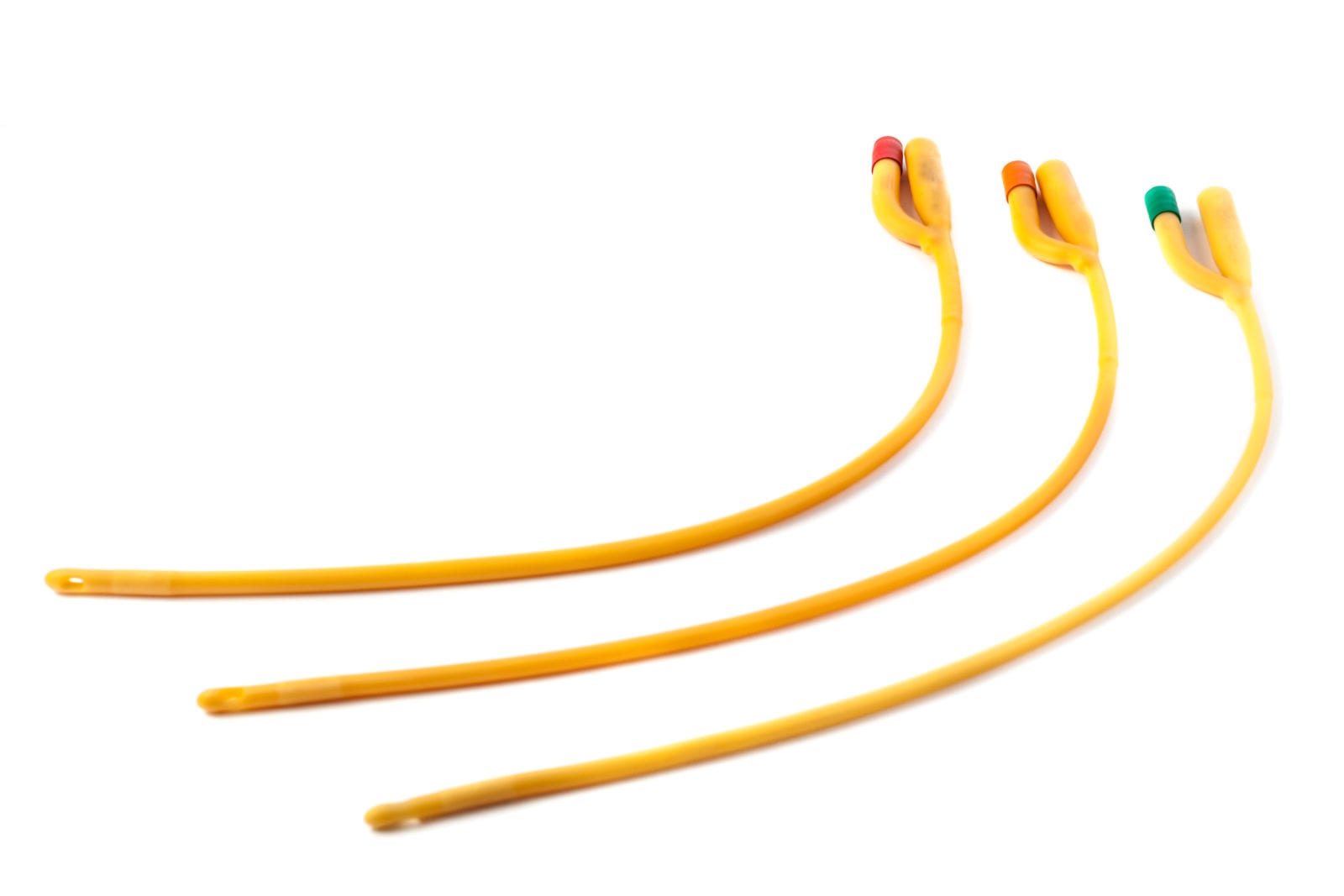
Intermittent catheters may look intimidating and scary at first glance. But looks are not everything. Once you get the hang of it, inserting it into your urethra will be a piece of cake.
If you are in need of one of these, a common question you may have is “Does Medicare cover Intermittent Catheters?” In this article, we answer this question in clear, plain English. You will also find the average costs of intermittent catheters, as well as other helpful info.
The short answer is yes; Medicare will cover the cost of intermittent catheters. But not 100% of the time. As is often the case with Medicare, certain conditions have to be met in order for Medicare to pay for your intermittent catheters. Below we look at what these are so you know what to expect.
Medicare covers intermittent catheters as they consider them to be a Prosthetic Benefit. What this means is they replace all or part of a body organ that isn’t working properly.
Medicare will cover up to 200 catheters per month as well as sterile lubrication packs. How many they cover depends on how many your doctor prescribes for you.
In order to get coverage, the catheters must be medically necessary. This will require a prescription from your doctor. Information on the prescription should include the item description (including the brand name and type of catheter), the quantity that you need each day as well as your diagnosis.
You’ll also want to get your catheters from a supplier who accepts Medicare assignment. If a supplier does not accept assignment, you may end up paying the difference between what they charge and what Medicare covers.
Once all the conditions are met, Medicare will provide 80% coverage for intermittent catheters’ costs. You will pay for the remaining 20% out-of-pocket.
Intermittent catheters can cost between $1 to $3 each. The price varies on the type of catheter that you need. This does not include the costs of lubrication packets.
An intermittent catheter, also known as a urinary catheter, is a medical device used to empty the patient’s bladder if they cannot do so themselves. This medical device usually comes with a drainage bag that captures the urine that is discharged from the patient’s bladder.
Intermittent catheterization involves inserting and putting out many catheters in a single day. Unlike indwelling catheters, which are catheters that stay on the patient for a long time, intermittent catheters have lesser risks of having infections, leaking, bladder spasms, and blockage.
A healthcare provider will insert the intermittent catheter inside the patient’s urethra. The urethra connects the bladder and the genitals. The catheter will be guided to the patient’s bladder. From there, the patient’s urine will flow through the catheter, leading to the drainage bag.
Once the urination process stops, the patient will need to move the catheter to check if they still need to release urine. Once the urinary bladder is empty, the patient can safely remove the catheter.
The process of doing so may sound scary, but it is a procedure that most patients adjust to without the help of their doctor or anyone. Intermittent catheters can help prevent UTI for those who have urinary incontinence.
Note: Medicare coverage changes all the time. And your specific coverage may vary from plan to plan for Medicare Advantage and Medigap plans. Always be sure to double check with your health care provider and/or Medicare insurance provider about what your plan covers and what it does not.
This article is part of our series on “What does Medicare cover?”
Also, you can check out other articles in this series including: Does Medicare cover car accident injuries?